Calls for safer sex and vaccination amid alarming increase in HPV-related cancer
Surge is in stark contrast to sharp fall in cervical cases
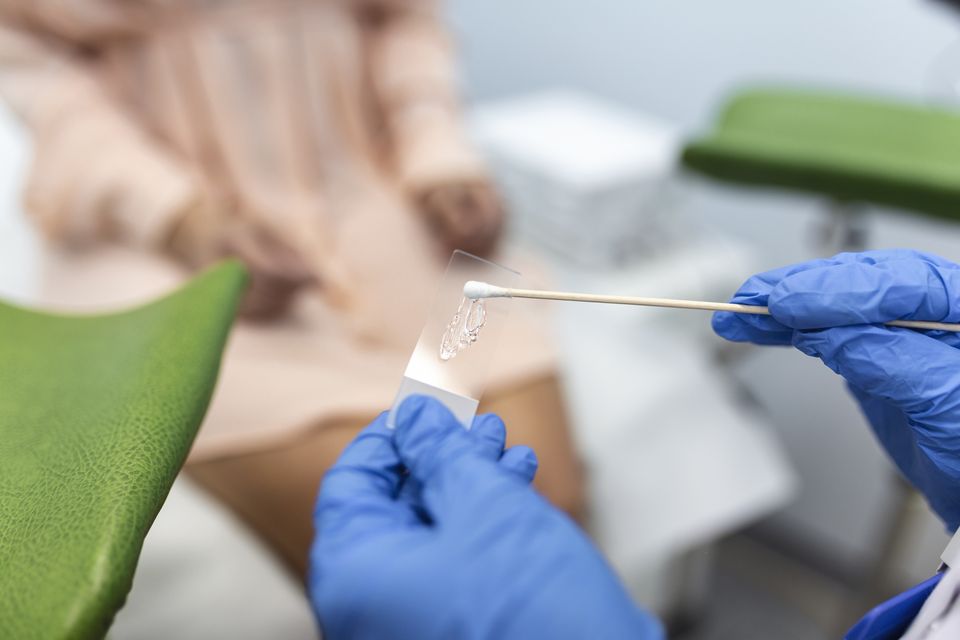
Cases of cervical cancer have declined, with the study saying this was down to free screening. Photo: Getty
A general increase in sexual-partner numbers has been identified as one of the reasons behind a rise in certain cancers in Ireland, according to a new report.
The study, by the National Cancer Registry of Ireland (NCRI), looked at the incidence of cancers associated with the human papillomavirus (HPV), a group of viruses known to infect the genital area, as well as the mouth and the throat.
While the incidence rate for cervical cancer is falling in Ireland due to screening, most other HPV-associated cancers are rising, according to the report.
It estimated that there are 641 cases of HPV-associated cancers diagnosed per year in Ireland, with 196 cancer deaths. Most of these deaths are potentially preventable by HPV vaccination.
Oropharyngeal cancers, which relate to the head and neck, are on the rise. Anal cancers are also increasing.
The report points out that HPV is now well-established as an important risk factor for cervical, vaginal, vulval, penile and anorectal cancers, as well as head and neck cancers.
It stated: “Almost all sexually active people develop HPV infections, and about half of these infections are with a high-risk HPV-type virus.
“These high-risk HPV infections are estimated to cause about 5pc of all cancers worldwide.”
Asked for some of the reasons behind the rise, a spokeswoman for the NCRI said: “International evidence has demonstrated that changes in sexual practices, including an increase in the number of sexual partners and engaging in unprotected sex, have contributed to the increase in HPV infections.
Read more
“Population growth and ageing also play a part. HPV vaccines are expected to reduce the prevalence of HPV infection and subsequent cancers.
“But the fall will be seen later than in cervical cancer as other HPV-associated cancers tend to occur at an older age.”
Head and neck cancers are more commonly diagnosed in a patient’s 50s or 60s, compared to 30s or 40s for cervical cancer.
Other HPV-associated cancers – penile, vulval and vaginal – are most commonly seen in the over-70s age group.
The report shows many HPV-associated cancers are diagnosed early. This is apart from head and neck cancers, the majority of which are diagnosed late.
Survival rates for most HPV-linked cancers continue to improve, but this varies by cancer.
CervicalCheck, the free screening programme to prevent cervical cancer, started in 2008. The positive impact on cancer incidence was seen almost immediately, the report said.
HPV vaccination was introduced for girls in first year of secondary school in 2010 and extended to boys in 2019. It is anticipated that this will reduce the incidence of all HPV-associated cancers in the long term.
Prof Deirdre Murray, director of the NCRI, said: “Cancers associated with HPV infection are potentially highly preventable. Vaccination and regular screening play crucial roles in preventing and detecting HPV-associated cancers early.”
The report said improving vaccine uptake is key to success, as is promoting safer sexual practices, and access to early detection and treatment.
Join the Irish Independent WhatsApp channel
Stay up to date with all the latest news